While bowels may not be the most glamorous topic, for many reasons our bowel system is critical for our health and wellness. As you may know this system is involved in the very important function of allowing us to excrete waste from our body. New research shows that 90% of our body’s serotonin is produced in the gut, showing us that much of our mood and mental health may also be related to our gut health.
The Gastrointestinal System (GI System): A Quick Overview
The digestive process starts when we first put food into our mouths. When we chew food in our mouth, saliva contains digestive enzymes, coats the food and helps aid the digestive process. The more we chew, the less work the rest of our system needs to do. So your childhood memory of hearing “chew your food and eat slower” is in fact true and important. We should eat slowly to allow ourselves to physically break down food in the mouth as much as we can and this also allows for the mixing of saliva and food. From our mouth, food then enters the esophagus. The esophagus is a tube that connects the mouth and the small intestine. From the small intestine, food moves into the large intestine. The large intestine is composed of three parts: the ascending colon, the transverse colon, and the descending colon. From the descending colon contents then move into the rectum, the last part of the GI tract before food is expelled from our body.
Our GI system is a complex one, formed by many different parts; lots of twists, turns, and length of organ for contents to travel through before being emptied from our bodies. This maze of a system is a fascinating one. As pelvic floor specialists within the world of physical therapy, we have the tools and skills to be able to help people who may be facing issues with their digestive tract. Some common conditions we see people for in physical therapy specifically related to the bowel system include incomplete bowel emptying, dyssynergic defecation, painful bowel emptying, and slow transit. These are just a few of the many dysfunctions under the umbrella of bowel dysfunction that we see – if you do experience trouble in this area and have been struggling to find an answer, speaking to a physical therapist may benefit you.
To touch upon these dysfunctions in a little more detail, let’s start with incomplete bowel emptying. Incomplete bowel emptying may occur when you are having a bowel movement but feel like you’re not able to fully void when going. Dyssynergic defecation refers to a muscular issue where the muscles in the pelvic region are not coordinated. When you are trying to void, the muscles in the pelvic region should open and lengthen but when they are dysfunctional, they may be contracting and tightening. This reversed movement can also be linked to incomplete bowel emptying. Painful bowel emptying is exactly what it sounds like. Oftentimes this can be resultant from rectal fissures, small cuts to the tissue lining in the rectal region that can lead to pain with the passage of stool. Slow transit is when the passage time for contents through your GI tract is longer than the norm. This can lead to constipation and feelings of discomfort or fullness in the abdominal region. In some cases, this may even contribute to decreased appetite due to the fullness and discomfort in the abdomen from lack of movement and ability to empty.

The Role of Physical Therapy in Treating Bowel Dysfunction
Now that we touch on some of the common dysfunctions we see with bowel dysfunctions, let’s talk about how physical therapy can help. In physical therapy, we can help provide education about posture, examine and treat the musculoskeletal dysfunction we find in this area and lastly, help retrain muscles that are dysfunctional.
Beginning with posture, at your first visit in PT we will assess your posture and help create a more efficient posture. When looking at posture, we will assess you in standing and sitting. For bowel dysfunction, we will specifically assess you in your regular toileting posture as this gives us great insight into how you’re aligning yourself during this function. Alignment during bowel emptying is critical as the position of your pelvis and hips affects the tension on a muscle called the puborectalis. The puborectalis muscle is a muscle that wraps around the lower rectum. Depending on the positioning of the pelvis and hips, the tension on this muscle changes. This becomes important in the process of defecation as a narrow angle of the puborectalis can lead to increased tension around the rectum potentially restricting movement of contents through this region. A wider angle of the puborectalis muscle creates a wider angle around the rectum allowing slack along the rectum and in turn allowing for easier passage of content through this area. Provided a wider angle between the puborectalis puts less tension on the rectum, this is the preferred or ideal posture for bowel emptying. To create this change we must keep the height of the knees higher than the height of the hips. Traditionally, toilets in the United States are quite high. This creates a sitting posture where the height of the knees is lower than the height of the hips or the height of the hips and the knees are the same. This height seat typically leads to a slumped back and tilting of the pelvis back. This creates narrowing around the tailbone and pelvic floor putting the muscles in a shortened position. In other parts of the world such as Asia, squat toilets are also standard. Squat toilets allow for placement of the feet on the ground on either side of the toilet and a low squatting position allows for the height of the hips to be lower than the height of the knees. This posture creates ease of movement of the low back into a slightly extended posture and creates more space and opening around the pelvic floor muscles.
To modify our current toileting posture, we can use an object to lift our feet off of the ground. One such way to do this is by using a stool called a “Squatty Potty”. This is a raised platform that conveniently fits under the toilet allowing for ease of use and accessibility. By raising the height of the feet off the ground, you’re able to assume a squat-like position. This places less stress on the puborectalis muscle. If you want to try this at home without making this purchase, you can also use a small step stool you may already have around your home to achieve a similar posture. I have also heard of patients getting creative and using other items around their household to elevate their feet. Any of these variations are okay to use.
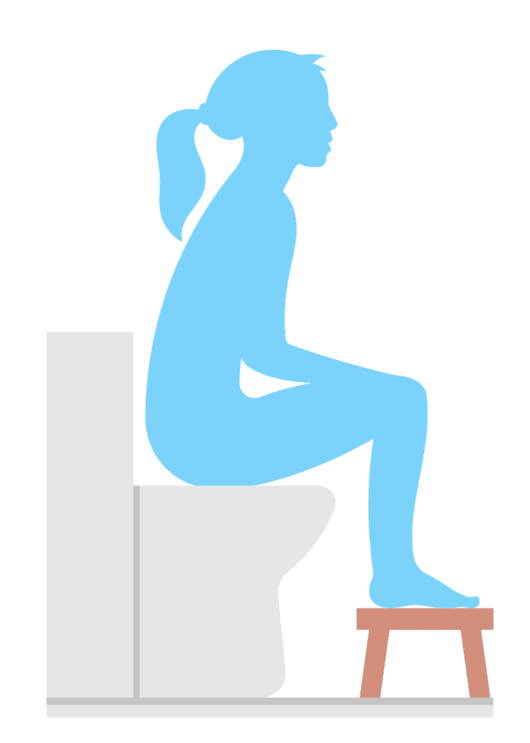
If you try using a squatty potty or any variation of this, it’s important to adjust your form when sitting and elevating your feet. Try rocking your pelvis forward and back a few times- this creates movement of your tailbone outwards and inwards. For those of you who aren’t familiar with how to move your pelvis, try placing your hands around your hip region. You should feel a large bony structure that wraps around- this is your pelvis. In the front of the pelvis you should feel 2 bony prominences, this is the anterior/ front portion of the pelvis. You can use these landmarks as pointers and direct them back and forth. This will create movement of the pelvis forwards and back. Find yourself in a slightly forwards tipped position. You should feel your lower back in a slightly extended position. This is ideal positioning – creating more space in the back part of the pelvis to allow for easier voiding.
If you are able to identify the pelvic region but are having trouble creating movement here you may have muscular restriction around the hips and pelvis that is contributing to this. A common challenge for patients with a squat position is they will have trouble with low back extension. The low back may feel stuck in a rounded position. Some of my go-to stretches for this type of dysfunction include stretching for the hamstrings. The hamstrings are a group of muscles that lie on the back side of the legs and have an attachment to the back side of the pelvis. Tightness here may contribute to the pelvis getting pulled back into a tucked position. To stretch this area you can try standing alternating toe touches- from a standing position alternate lifting your leg upwards towards the opposite extended arm. Keep alternating sides for 3 sets of 10-12 repetitions. You can also try seated toe touches. The key with this exercise is to keep the low back in slight extension. You may not be able to touch the toes with the low back in extension so try wrapping your arms around the back of the thighs while drawing your chest forwards in the seated position. Hold for 15 seconds 3x. This mobility work may help increase your pelvic range of motion but best practice is to always seek an evaluation from a practitioner if you are experiencing dysfunction.
Retraining and Strengthening the Pelvic Floor
In addition to assessing and correcting posture, physical therapists can also examine other parts of your musculoskeletal system. We have the skill set to be able to assess the fascia in the abdominal region. Fascia refers to a layer of connective tissues that envelopes our bodies. The deepest layers of fascia that envelop our organs help suspend our organs within their cavities. Like muscular tightness, fascial tightness can create limited or dysfunctional movement patterns and can contribute to bowel dysfunction and/or pain. Physical therapists can assess fascia using their trained hands and can manually work on this tissue to ‘untangle’ it and can also lead you through exercise to be able to maintain movement in these areas. We can also use movement analysis to assess your mobility through your trunk, pelvis, and hips area. Restricted range of motion in these areas can create dysfunctional movement patterns of the tissues and organs within our bodies. We can use guided movement and targeted exercises to help create improvements in our range of motion.
Like fascial restriction, we can also assess the pelvic floor muscles. The pelvic muscles can be examined externally or internally if indicated and with consent. Typically these exams are performed manually. A therapist can apply pressure to the different layers of pelvic floor muscles to assess for areas of restriction. For muscle tightness, exercise or manual therapy can be used to decrease this tension. Exercises targeting lengthening of the pelvic outlet can be instructed. One example of this is the ‘happy baby’ yoga pose. This pose allows for opening through the sits’ bones area and allows for lengthening in the area. An example of a manual therapy technique that can be used to treat areas of tightness include trigger point releases. This is where the therapist applies sustained pressure to a tight area allowing it to slowly release. During this manual exam, a therapist can also examine muscular strength by having you perform a pelvic floor muscle contraction. For weakness, exercises targeting the pelvic floor can be administered, while for overactivity of the muscles, training to decrease tension generated in this area can be performed. If during the exam it’s found that a person is unable to adequately coordinate pelvic floor movements, then re-training of the muscles is appropriate.
For re-training of the pelvic floor muscles, we can use biofeedback. Biofeedback is a technique that is used to help create a stronger mind-body relationship. There are many forms in which feedback can be administered. One possible way is manual biofeedback, this is where the therapist can use tactile feedback to help you develop increased awareness of the muscles. There is also digital biofeedback where a sensor or pad can be used to help create awareness of the relationship between muscular movement and the action that’s being generated. The sensor can be placed intra-vaginally or intra-rectally and its connection to a device allows for you to visualize whether you are contracting, relaxing or lengthening the muscles in the pelvic region. The pads can be used as well, these are especially useful in cases where a patient is symptomatic with pain in the region. The pad placement is on the external pelvic muscles and works similarly to the sensors where they allow for visualization for movement of the muscles in the pelvic region.

Conclusion
The variety of techniques for the assessment and treatment of bowel dysfunction is vast. If you’ve been experiencing bowel dysfunction or have tried using medication or making changes to diet but haven’t touched upon physical therapy – this may be for you. With a physical therapy assessment, you’ll be able to better understand how posture, fascia, muscular tightness, muscular weakness, or muscle coordination may be impacting your symptoms. This system is complex and when dysfunction arises it can be daunting but we hope after reading this today, you feel empowered with some knowledge and tools to help you navigate your health journey.
Pelvic Floor Disorders and Treatment
— Beyond Basics PT | Pelvic Floor Therapy NYC.
Frequently asked questions on Bowel Dysfunction and Neurogenic Bowel Disorders
What is bowel dysfunction?
Why is gut health important for overall wellness?
What factors influence healthy bowel function?
Maintaining healthy bowel function involves a combination of factors:
- Diet: A high-fiber diet promotes smooth bowel movements.
- Hydration: Drinking enough water softens stools, reducing constipation.
- Exercise: Physical activity stimulates the digestive system.
- Gut Microbiome: A balanced gut microbiome supports regular digestion.
Can bowel dysfunction affect bladder control?
What conditions can lead to both bladder and bowel dysfunction?
Common causes of dual dysfunction include:
- Neurological Disorders: Conditions like multiple sclerosis and Parkinson’s disease.
- Chronic Conditions: Diabetes can cause nerve damage that affects both systems.
- Physical Trauma: Spinal cord injuries often result in neurogenic bladder and bowel dysfunction.
What are the symptoms of dual bladder and bowel dysfunction?
- Urinary Issues: Incontinence, urgency, frequency, and incomplete emptying of the bladder.
- Bowel Issues: Fecal incontinence, constipation, urgency, and difficulty with bowel movements.
How are bladder and bowel dysfunctions diagnosed?
- Physical Examinations: To assess symptoms and nerve function.
- Patient History Review: To identify underlying conditions.
What therapeutic options are available for managing bowel dysfunction?
- Medications: To regulate bowel movements.
- Physical Therapy: Strengthening muscles involved in bowel control.
- Biofeedback: Training to improve awareness of bowel control.



